Even before you know you’re pregnant, folate, or folic acid in its manufactured form, is performing its role of supporting your baby’s development. It plays a significant role in the formation of your baby’s neural tube – the structure that forms in the first month of life that eventually becomes your baby’s spinal cord and brain.
Together, these will form your baby’s central nervous system, which will act as the control centre for your baby’s whole body, and provide the foundation for all future growth, development, and normal functioning later in life. Since there is a well-established relationship between maternal folic acid intake and development of the neural tube in the young foetus, it is easy to see why taking a supplement of folic acid is strongly recommended during early pregnancy.
An adequate intake of folic acid has been shown to reduce the risk of neural tube defects (NTDs) including spina bifida. This condition results from the spinal column not closing properly, leaving the spinal cord exposed and potentially causing developmental problems.
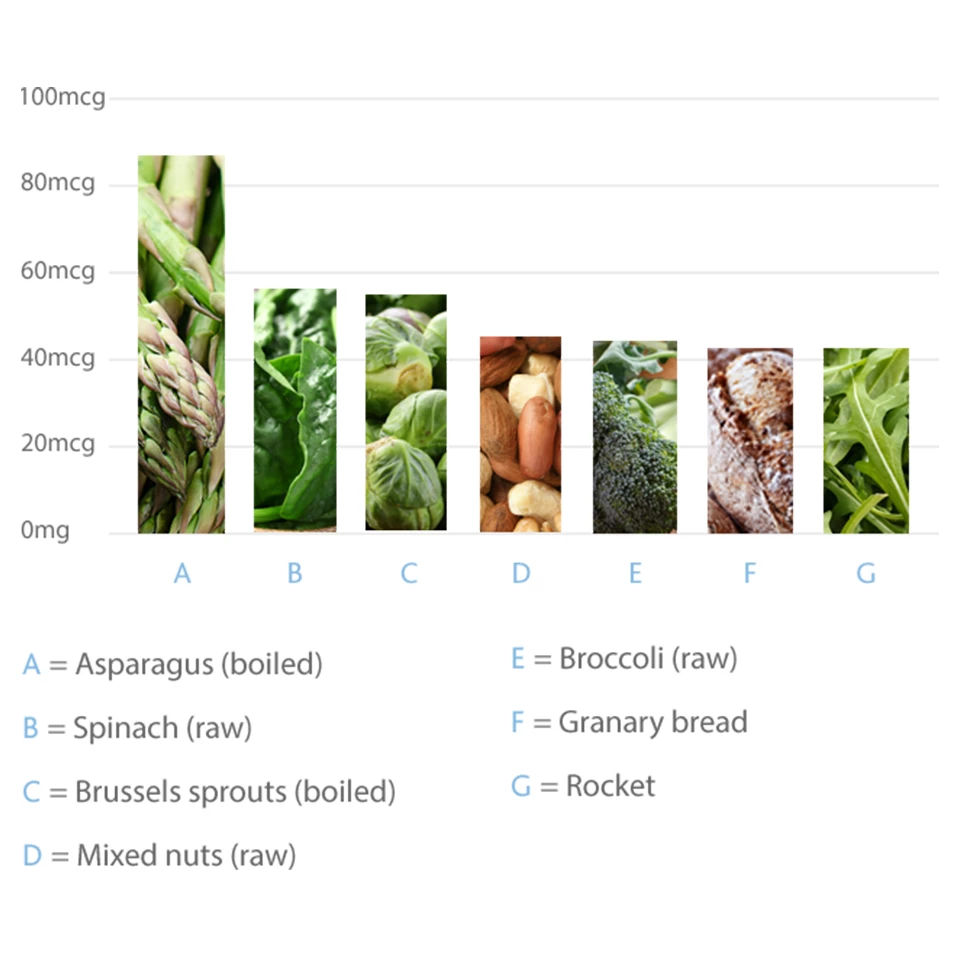
Although folate is present in many foods, it’s difficult to get sufficient levels from your diet. Taking a daily supplement means you can be sure you’re getting the amount you need to support your growing baby.